This section is the common path on Map 2 for a physiologically dependent patient who refuses detoxification. It is preparation for issues of ongoing therapy in Section 27, Map 5.
If a person is currently physiologically dependent on alcohol, there may be very little you can do for him/her beyond pressuring for detoxification [ Section 7 ] or arranging for an intervention [ Section 13 ].
However, it is possible to work toward detox within a therapeutic setting. In fact, the therapeutic process may provide the person’s primary – or only – opportunity for change, short of a medical collapse, major accident, or personal failure.
There is always an issue regarding how much use any physiologically dependent person can make of the normal treatment process – or whether the usual treatment process can be modified for a particular patient in order to make it more helpful to him/her. You might have more impact on such a person if you have frequent sessions and s/he engages in some adjunctive care activities. You should not expect much movement relative to the person’s other psychological or practical issues, because he/she probably can’t focus on them effectively.
The decision about whether to continue working with a physiologically dependent patient is not easily made. Keeping the person in treatment could be interpreted as approval or acceptance of his/her drinking, or as admission that nothing can be done about it. Sending the person away could give the message that the problem is untreatable, or the person is unimportant. This could actually exacerbate his/her alcohol use [especially if rejection is a psychological issue], and at the same time reduce accountability for drinking.
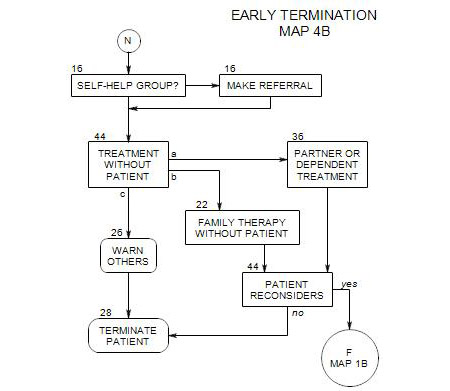
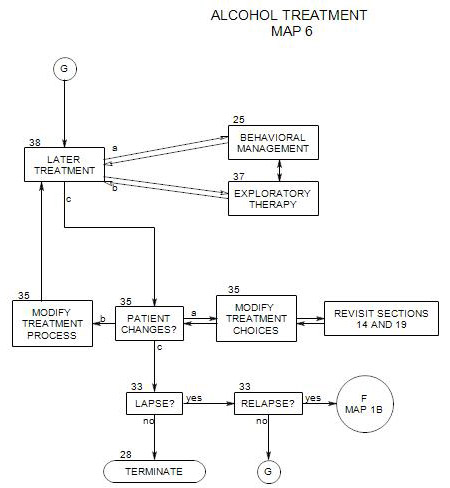
If the patient won’t continue, or if you decide that further work with him/her is unlikely to have any noticeable effect, you can continue treatment without the patient [ Section 44 ] or terminate the case [ Section 28 ].
39a. Terms for Continued Treatment
The ground rules for continued treatment must be clear. The patient must not drive drunk to sessions, no matter what. This must be understood by the patient and adhered-to. He/she can get a ride to treatment, take a taxi or public transportation, or walk. Some patients may have difficulty with this rule. Their judgment about their own drinking may be compromised, either with regard to their drinking or to its effects. “I only had two little ones before I came. I’m fine.” Failure must be handled with some kind of immediate correction, lest the patient have an accident on the way home from treatment or consider it acceptable to come in the same state on another occasion. Having sessions early in the day may be helpful to some patients.
Depending on the patient, the ground rules for continued treatment could also include that he/she –
- comes to sessions sober if possible.
- comes several times per week.
- tries attending a self-help group.
- comes to sessions no matter how hung over.
- doesn’t attempt to self-detox without consulting a professional first.
39b. Process
Some differences in treatment can be predicated on the patient’s stage of change [ Section 40 ]. For a patient who is in a contemplation or preparation stage, it may be the only place to express ambivalence about drinking – especially the negative effects of alcohol. It may be the only place he/she can plan for sobriety without taking immediate action or facing the scorn of others who can’t tolerate his/her ambivalence and delay.
This is the kind of situation for which motivational interviewing [ Section 24 ] was designed. The therapist should be empathic, help the patient articulate goals, explore any ambivalence the patient may have, roll with the patient’s resistances, and support patient self-efficacy. The overall goal is to help the patient find his/her own way to move on to the action stage.
If the patient is in the precontemplation stage [full denial], then the goal of detoxification becomes both more important and more elusive. The person’s lack of ambivalence about drinking may make him/her a greater risk in many ways and at the same time less willing to consider that risk. The additional goal of moving him/her to the contemplation stage is both important and difficult to pursue without driving the person from therapy. Here again, motivational interviewing may be helpful.
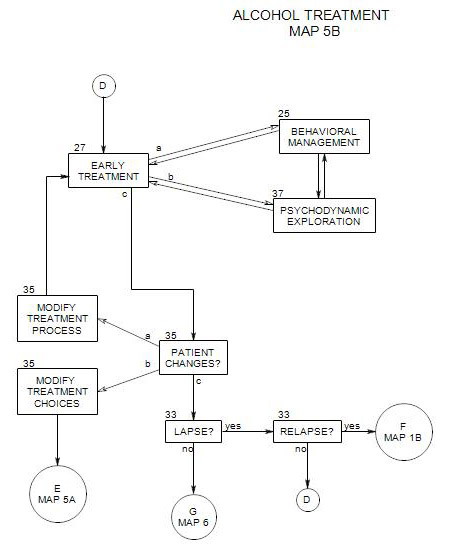
Even though it may be fully effective, the therapist may want to introduce aspects of psychotherapy at this point – choosing a primary form of care, suggesting adjunctive treatments, and making use of some techniques of early treatment [See Map 5A]. Partial benefit may be better than none, and may actually encourage movement toward recovery.
39c. Next Steps
Sooner or later – often later – a physiologically addicted person must deal with the addiction or risk serious consequences. Some people may be able to cut back on their own. Most have to go through detox and rehab in order to make any change in their lives. Once a person has dealt with his/her physiological addiction, outpatient treatment can focus more effectively on alcohol management and the other issues the person needs to deal with.
Some patients may never get to the point of detoxification. In that case, little can be done for them, and the therapist may eventually need to consider treatment without the patient [ Section 44 ] or even termination [ Section 28 ].
If you decide to continue treating a patient despite alcohol dependence or abuse, subsequent steps follow Map 5A. In that case, continue to press the person for abstinence in sessions, and recommend adjunctive care that supports reduced drinking or abstinence. This could include family involvement [ Section 22 ], self-help group attendance [ Section 16 ], an alcohol education series [ Section 31 ] and medications that reduce alcohol interest [ Section 19 ].
44. Treatment Without the Patient
This issue can come up in several places in treatment, when the identified patient refuses to, or is unable continue, and his/her drinking remains a serious problem for self and others. Family therapy that includes the patient is discussed in Section 22 and partner therapy in Section 36.
The issue here is treatment for others in the family of an alcoholic patient, when the identified patient [IP] is unwilling or unable to come for therapy. The IP may be an active alcoholic or somewhere in the recovery process. The problem is to decide whether something can still be done to help the IP and/or others in the patient’s family. In this case, it is important to keep your therapeutic goals in mind, and expect that the goals may change over time. Broadly speaking, therapeutic goals can be focused on the IP, others in the family, or the family as a whole.