7. DETOXIFICATION
- This section follows Section 6, when a determination has been made that a patient is physiologically dependent and in danger. Detox is followed by the choices on Map 3.
This is a medical procedure for temporarily removing a person’s physical dependence on alcohol, while at the same time minimizing the side effects that withdrawal can produce. It is temporary in that it is an effective beginning for a process that can be ended any time that the person returns to drinking. The procedure requires total abstinence and ongoing monitoring for withdrawal symptoms, which could range from mild to severe. Detox time varies, typically lasting from five to seven days.
7a. Withdrawal
A physiologically dependent person who abruptly stops using faces a variety of symptoms due to the changing level of alcohol, as well as the appearance of conditions that have been created by alcohol use and the reappearance of symptoms that have been masked by it.
Minor symptoms during detoxification include irritability, anxiety, rapid mood changes, fatigue, trouble sleeping, shaking, confusion and depression. Physiological reactions include increased blood pressure and heart rate, high temperature, sweating, headache, loss of appetite, nausea and vomiting.
More serious withdrawal symptoms can include chronic confusion, delirium, hallucinations and seizures. Exact symptoms can’t be predicted for a person’s first withdrawal, and they change from one to the next. Because symptoms can’t be predicted and can be serious or even fatal, medical management is extremely important.
Repeated withdrawals can lead to increased severity of symptoms, increasing the risk of relapse, brain damage, permanent changes in body chemistry, and increased risk of death during withdrawal.
7b. Detox
The detox process is designed to manage symptoms of abrupt abstinence and treat any other issues that become apparent during the process. Medical support includes the use of multiple vitamins to replace losses from drinking and benzodiazepines to lighten symptoms. During this time, the person must be closely monitored. Alcohol and anxiolitics are both central nervous system depressants, and the drug substitutes in part for alcohol during detox, reducing side effects. However, if the person continues to drink, the drug and alcohol can compound to create even more serious problems and possibly death.
7c. Getting the Patient to Go to Detox
If the patient recognizes his/her dependence on alcohol and is willing to go for detoxification, the discussion moves on to the various options, based on treatment availability and patient needs. If not, several choices remain:
- Explore with the patient his/her current drinking behavior and symptoms, to understand better whether he/she is really physiologically dependent.
- If the person is clearly dependent and admits it, try to understand his/her reluctance to go and convince him/her to go, based on symptoms
- Examine together the dangers of continued physiological dependence [Section 6], and use the dangers as leverage to convince him/her to go.
- Suggest an alcohol education series [ Section 31 ], so the patient can learn more about the effects of continued drinking.
- Offer a cooperative intervention, or arrange a confronting intervention [ Section 13 ].
- Continue to treat the patient for other psychological issues, with a further agenda of getting him/her into detox in the future [Map 5A]
- Terminate the patient [ Section 28 ] and warn others who might be impacted by him/her if appropriate [ Section 26 ]
7d. Treatment Settings
Detoxification can be carried out by medical and psychotherapeutic staff in a variety of settings. The range is roughly the following, in order from most intense and restrictive to least:
- Specialized inpatient hospital
- General inpatient drug and alcohol treatment center
- Partial or day hospital
- Drug and alcohol clinic
- Private medical office
A thorough listing of treatment options at this point should also include two others:
- Outpatient psychotherapy without detox
- No treatment
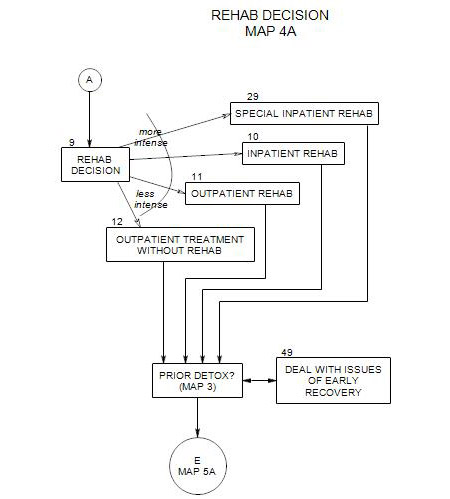
The choice of detox settings depends on treatment availability and patient characteristics and needs. Following are brief descriptions of types of treatment settings, followed by a consideration of some patient issues that could affect placement.
GENERAL INPATIENT DETOX
This is generally the treatment setting of choice, involving supervised inpatient care, medication, and intensive individual and/or group counseling.
Length of stay in the detox facility is dependent on
- level of alcohol dependency;
- the nature of the substances (including alcohol) on which the patient is dependent;
- other presenting medical issues;
- insurance coverage, when applicable.
The usual length of inpatient alcohol detox with no complications or concomitants is five to seven days, but may it require up to two weeks. Patients are re-evaluated regularly to assess their progress, regulate their medication, and determine whether they need additional inpatient care.
SPECIALIZED INPATIENT DETOX
This may be necessary if the patient presents special risks that a regular detox facility isn’t equipped to handle. These could include the possibility of medical complications or the presence of a serious illness, such as diabetes or seizures, which is affected by alcohol use and/or by the withdrawal process. A person with an untreated psychosis may need staff with special knowledge and skills. People who are suicidal or potentially violent need additional management for physical safety.
In many cases, it won’t be possible to determine the patient’s full diagnostic picture at the time of referral. It also may not be critical. If the patient seems intact enough to handle a standard detox program, that is where he/she should go. If there are unrecognized complications, the staff at the facility will have an opportunity to sort out the picture and refer the patient on if needed.
OUTPATIENT DETOX
Treatment can be carried out in a partial or day hospital setting or in a clinic or private medical office. The patient has to commit to abstinence, and the transition to sobriety is eased with medication, typically Librium, vitamin supplements, and calming interventions such as acupuncture.
A disadvantage is the lack of control of the person’s daily life, by comparison with inpatient treatment. This may be compensated for by attempting to manage the person’s time through use of family, self-help meetings, counseling and education and a sober-support-person. Family and friends may also be enlisted to help the person avoid drinking, if they are available and able to help.
Because there is less physical control of the patient, there is greater possibility for early relapse – during the detox process itself. When that happens, the process must be begun anew or temporarily abandoned.
NO DETOX
A professional should not assume the risk of recommending that a person detox him/herself or continue a physiological dependency without detox. Either path is full of dangers. Self-detoxification leads to risk of seizures, delirium tremens [DT’s], heart attack and other medical consequences. In extreme cases, it can be fatal. Continued physiological dependence brings a wide range of short- and long-term risks, as indicated in Section 6.
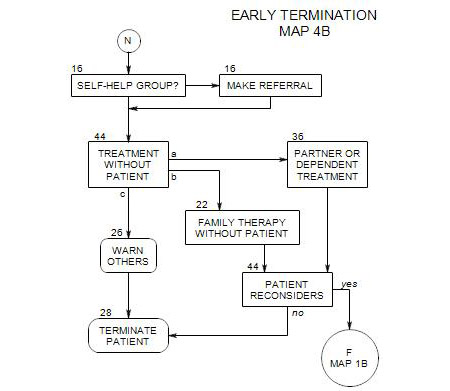
However, the patient may refuse to detox. In this case, the next step is to decide whether to press for detoxification through having an intervention [ Section 13, Map 2 ], or to continue working with a patient who is physiologically dependent [ Section 39 ].
If the patient refuses further treatment, termination may be inevitable. However, you can in some cases continue to work with the patient’s family or network of friends and co-workers [ Section 22 ]. If not, and your patient poses a danger to self or others, you may have a responsibility to notify others about it [ Section 26 ].
7e. Making a Detox Plan
A wide range of patient characteristics can influence the choice of a detox plan. They all need to be considered, but their relative salience will vary from patient to patient. Major issues include
- How to keep the patient medically safe
- How to manage the patient’s discomfort – and how much to expect
- How to keep the patient from drinking during detoxification
- How to transition the patient out of detox and into rehabilitation
PATIENT SYMPTOMS
Very severe symptoms include untreated or ineffectively treated psychoses, or history of violent behaviors. These may require special patient management and specially trained staff.
Severe symptoms include serious anxiety or depression, hallucinations, blackouts, a history of seizures, a history of several prior detoxifications, a history of binge drinking. A comorbid psychological disorder that is under control through medication. These require ongoing patient monitoring by a trained staff. The more and longer that a person has been drinking, the greater the need for medical management during detox.
Less severe symptoms include irritability or milder forms of anxiety or depression.
TREATMENT HISTORY
The patient’s previous treatment history can be an effective guide to what may or may not work in the future. If the patient has been able to detox in outpatient treatment in the past, it might work again. If a particular treatment facility has been comfortable or effective, it might be good to return the person to that place. If prior detox has been ineffective, a change may be indicated. Because the detox facility almost universally makes the rehabilitation referral, it is important to consider the likely rehab referral when making the detox choice.
PATIENT ATTITUDE
How badly does the person want to detox, and how will attitude affect treatment in the various settings available? A patient who refuses inpatient detox may be ready for outpatient detox. A person with little drive to get sober may need the additional structure of an inpatient facility.
FINANCIAL ISSUES
There are a range of costs associated with detox, including the cost of the treatment, temporary loss of income if the person is treated on an inpatient basis, and possible loss of job if s/he is away from work for a period of time. Generally speaking, privately funded inpatient facilities are more expensive and may not accept insurance; publicly funded facilities are less expensive and accept insurance, and outpatient detox is less expensive than inpatient.
PERSONAL RESPONSIBILITIES
If the person has been able to continue the responsibilities of daily life and it appears that he/she will be able to continue them throughout a detox program, s/he may press for outpatient treatment. However, for a person to attempt to manage normal responsibilities while experiencing a severe detox might be to expect too much.
TEMPTATIONS OF EVERYDAY LIFE
It may pay to remove the person from the settings where heavy drinking has been taking place. It may be too much for a person to undergo the stresses of an outpatient detox program while his/her usual form of stress relief is still available but not allowed.
SUPPORT SYSTEM
For any treatment program, the people in the patient’s family and daily life are important components of the treatment. The patient may need to get away from pressures by others to drink, or to get away from the attitudes of others that serve as triggers for drinking. On the other hand, a supportive family or network can reduce the need for full-time medical management for some patients.
7f. Making the Referral
Generally, you
- negotiate with the patient re detox
- select a facility or a path to get the patient there
- make the referral
- arrange to get the patient there.
Once you have determined that a patient needs detoxification, you will need to make the referral based on the local options available to you. This could include
- Referral through a screening agency
- Direct referral
Because the moment of referral is often emotionally charged, the referral process should be as efficient as possible. You should know in advance what the process is and how to do it effectively.
At the treatment facility, they will
- verify the patient’s need for detoxification
- carry out the process, if they think it is needed
- refer the patient on for rehabilitation or outpatient therapy.
REFERRAL THROUGH A SCREENING AGENCY
In some places, the most efficient way to send a patient to detox is through a local hospital emergency room or other screening facility. Once there, the patient is interviewed by a staff member, who will make the determination of need and find an appropriate and available treatment facility.
THERAPIST REFERRAL
Here, the responsibility for getting your patient to a treatment facility rests with you. Your effectiveness will depend on your knowledge of the treatment options, contacts within the available facilities, and time in making the contacts and getting the person to the chosen facility.
SELECT THE PROGRAM
In selecting a hospital for detoxification, several things should be considered:
- Whether the patient’s insurance and managed care companies accept the chosen facility as a provider. This information is better obtained from the hospital, but the patient’s insurance company may have a list of approved facilities.
- Whether there is an associated rehabilitation program. Ideally, both inpatient and outpatient rehab programs would be affiliated with the hospital, to allow for continuity of follow-up treatment.
- Aftercare referral practices, e.g.: whether the program refers back to the professional who originally referred the patient to them.
MAKE THE REFERRAL
It helps to be familiar with the facility, the program, the personnel, and the procedures for admission. This will help you gain patient compliance and cooperation of the facility.
Ideally, preparation should be made with the hospital before you see the patient. Having a list of resources readily at hand is very important at this point. Call the admissions department, explain that you have a patient in need of detoxification, and ask if they have a bed available. If they don’t, call the next hospital on your list. Sometimes one facility will help you locate an available bed at another facility. If you are not prepared in advance, it may be necessary to make the calls during the therapy session in which the patient decides to go.
SELF REFERRAL
At many treatment facilities, it is possible for a patient to walk in without a professional referral. A major limitation of this approach occurs when the person can’t be seen immediately at an outpatient office or clinic, or there is no room at an inpatient facility. This can be discouraging, especially to a person who is ambivalent about the process. A better route is to call ahead and verify the availability of services.
7g. Getting the patient there
Next the patient will have to be convinced of the need to be admitted. How you handle this, and your likelihood of success, will depend on a number of factors, including the patient’s readiness for change [ Section 47 ]. It will be more difficult to convince a person in the contemplation stage than someone in the preparation or action stage.
In your office, explain the reasons that detox is the most reasonable step right now: the severity of his/her illness, the ways that the patient’s life and the lives of others are threatened, the danger of stopping without medical supervision and the need for a secure environment, etc. See Section 6 for help with this.
If you want to resume treatment with the patient once the alcohol issues have been brought under control, it might be good to tell the patient, and to invite him/her to return to you later.
If possible you can get a release from your patient before he/she leaves for the treatment facility, then contact the intake staff as soon as possible after s/he gets there. If not, the staff may arrange to obtain a release to talk with you. Then you can let them know that the patient was seeing you for outpatient treatment prior to intake, that you are prepared to keep in contact with him/her by telephone while he/she is there, and that you are available to see him/her again upon discharge. When staff are not available for individual treatment, it may be possible for you to have regular telephone sessions while he/she is there.
If you are uncertain about being able to convince a patient to go to a hospital willingly, you may want to enlist the support and pressure of friends, relatives, and co-workers. Threats of legal action may be effective, and it may help to have others present to assist in this process. In its more powerful form, the use of pressure from significant others is called an “intervention”; see Section 13 for more on this.
Once the patient is prepared, it is critical that he or she not wait. Arrange for him/her to go there immediately.
The patient should be accompanied to the hospital. Some facilities may provide transportation; or you can call a relative or friend of the patient to do the driving. If no one else can be found, go yourself. Under no conditions should the patient drive him- or herself. A patient who is put into a taxi or his/her own car will often end up in an accident or a bar.
The hospital will need to do their own screening regarding appropriateness; and they will want to speak to the patient, e.g., regarding insurance or procedures. A relative may have to provide the information, if the patient isn’t able to. If the patient is covered by managed care, the managed care company may have to pre-approve the admission. As the professional referral source, you will be an invaluable source of information on the patient’s history and present clinical state.
7h. What Follows Detoxification
This depends on a number of factors:
- hospital policy
- the patient’s need for rehabilitation
- the patient’s willingness to go for rehabilitation
- your alcohol credentials and knowledge
- your level of involvement in the process and your wish to continue with the patient
- the patient’s wish to return to work with you
If you have sent the patient for alcohol treatment because his/her dependence or abuse was interfering with treatment, then the ideal thing is for the patient to continue with alcohol treatment – in whatever form is needed – until s/he is sufficiently recovered that psychotherapy can be helpful. These choices are shown on Map 3. A patient who returns to therapy too soon after detoxification is at greater risk to relapse.
Patients should be reassured that detoxification is only the first stage of the work, and that further treatment will be available in order to help them deal with sobriety and other issues that have contributed to the felt need for alcohol.
If the patient is returned for continuing psychotherapy without rehabilitation, the next section is Section 12. If s/he returns after rehabilitation, then the next section is Section 49.