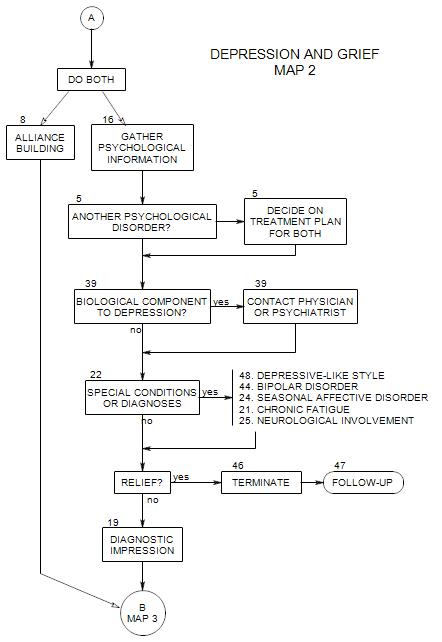
SECTIONS: 5 | 8 | 16 | 19 | 21 | 22 | 24 | 25 | 39 | 44 | 46 | 47 | 48
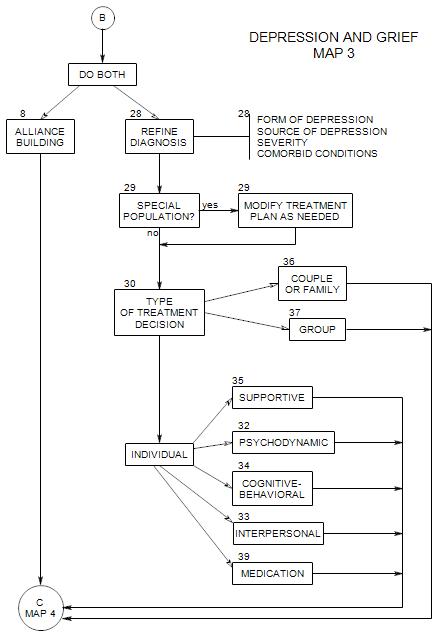
SECTIONS: 8 | 28 | 29 | 30 | 32 | 33 | 34 | 35 | 36 | 37 | 39
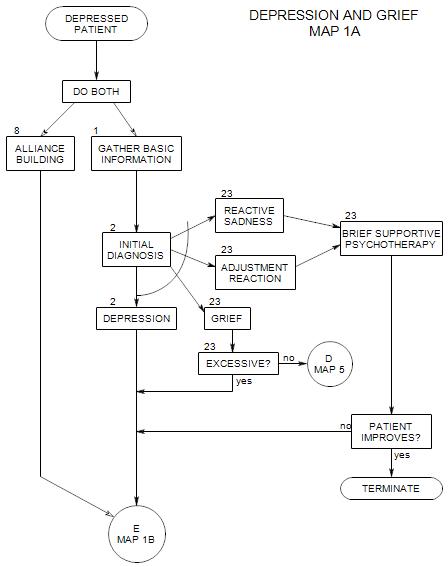
This section appears at the top of Map 1A.
Here you must pursue the information that you think will help to get the treatment started most effectively. You have very limited time in the first session, and the way that the first session goes will determine whether the patient continues, and whether he/she continues with you.
You need to
- identify and evaluate the depression
- decide on a level of care
- gather some practical information
- begin the treatment process
What follows is an abbreviation of material in the New Patient map, as applied to a depressed patient.
Start by asking about the presenting problem. It is the patient’s reason for coming in and of greatest importance. If the problem is depression, ask about that. If it is something else, and you also see that the patient is depressed, you will have to choose between the two or find a way to ask about both. This is discussed in Section 2.
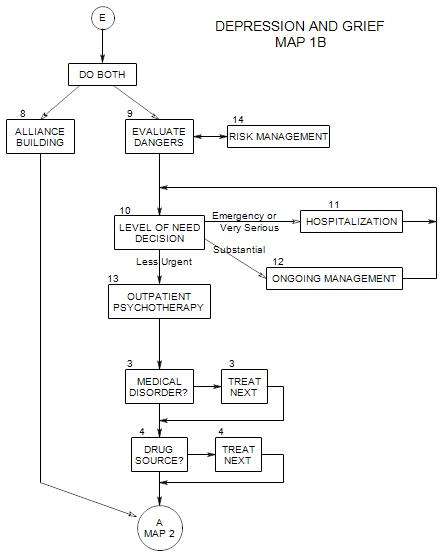
Depressed people present risks to themselves and others. You need to find out what risks this patient presents with, and how great those risks are. This is discussed in Section 9.
If the person appears to be depressed, a variety of special dangers need to be considered, including:
- suicide
- neglect of health or safety. This could involve not eating, overeating, or eating badly; lack of cleanliness; ignoring safety precautions; and in general not caring about things that matter for normal living.
- passively irresponsible behaviors: just not…going to work, getting out of bed, watching the children carefully enough, etc.
- not coming for treatment, because they just don’t feel up to it.
- being unable to work toward feeling better. Giving in to the depressive feeling.
The person may or may not tell you all you need to know in order to assess safety. This is a point where you should consider getting information from family members or others who are responsible for him/her.
Ask about timing:
- When the patient’s depression started, and whether it has been consistent or variable. If it has varied, ask about any patterns that the person is aware of.
- Ask why the person is coming to you now. This may relate to severity of depression, sense of failure on his/her own, or something else.
Ask what the patient wants and expects from therapy. There is a reason that he/she came to you at this time. What is it? How can you help?
Work on the patient’s alliance with you, and with treatment. Treatment is a collaborative effort, and the patient has an active role. Help him/her begin to define it and to work actively with you. For more on this, see Section 8 and New Patient Section 11.
Find out about the patient’s availability to come to sessions, and decide on an initial plan for treatment. This could be as simple as deciding to meet for three more sessions, to see whether you can be of help.
Work out your financial arrangement with the patient. Again, this may be a temporary arrangement. See New Patient Section 19.
Confidentiality discussion. It helps a patient feel safe to know that his/her secrets won’t be told to anyone without his/her permission and awareness. You must also establish the limits to confidentiality:
- risk of hurting self or others may mandate that others be warned and/or enlisted to help.
- need to communicate with insurance and managed care companies.
For more on this, see New Patient Section 25.
You can discuss the pros and cons of contacting others who can help you understand him/her: family, physician, referral source, friends, a hospital, etc.
If you decide together that it would be helpful to contact one or more of them, ask for their addresses or phone numbers. Have the patient sign a release so you can get the information you need.
If the patient was recently hospitalized, ask about the reason, name of the hospital, the dates, the length of stay, what was done, etc. Get a release to contact the hospital for information.
Ask if the person was ever hospitalized for depression in the past.
Make a note of your reaction [countertransference] to the patient. If the patient is depressed, you may find yourself feeling depressed, anxious, or annoyed and rejecting.
Note that the discussions of asking about depression and working on the alliance have been divided into Sections 1 and 8 for conceptual clarity, but that you must deal with both together. If the patient is coming to you for depression, both must be dealt with in the first session. Also note that, although we have shown these two issues to be part of the first session, they clearly will continue into later sessions as well.