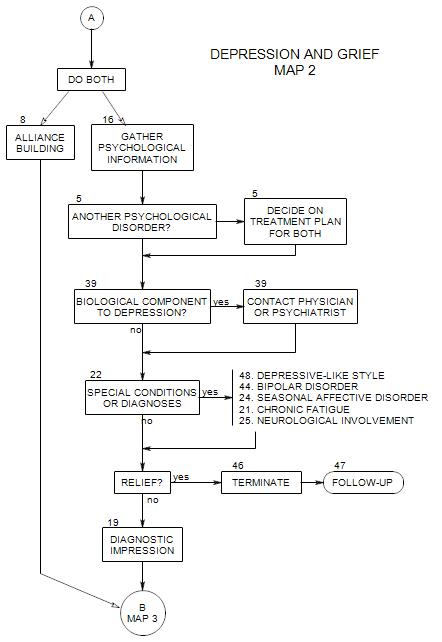
SECTIONS: 5 | 8 | 16 | 19 | 21 | 22 | 24 | 25 | 39 | 44 | 46 | 47 | 48
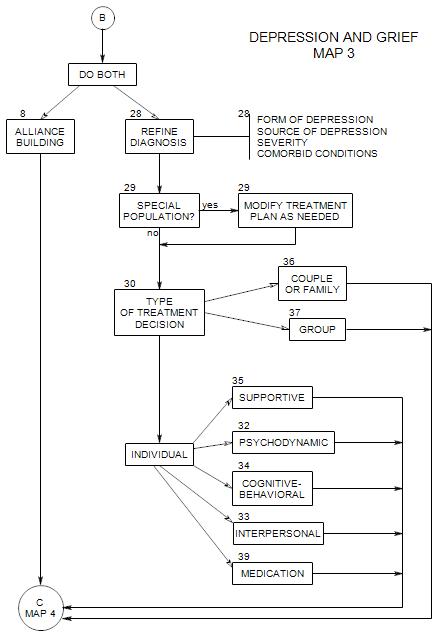
SECTIONS: 8 | 28 | 29 | 30 | 32 | 33 | 34 | 35 | 36 | 37 | 39
-
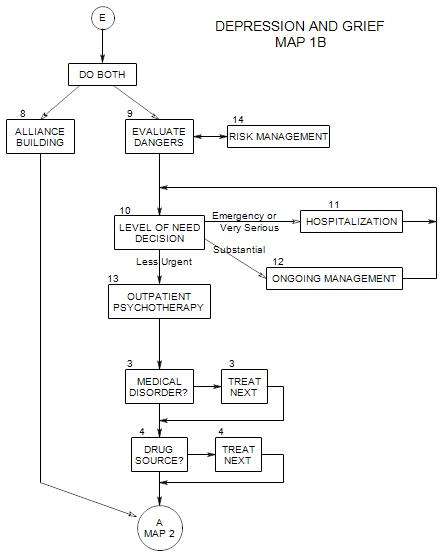
Follows Section 10 on Map 1B
Hospitalizing a patient is important to consider if the risk is great or the patient’s judgment is compromised [ Section 9 ] or if the patient’s need is very great or at the level of emergency [ Section 10 ].
11a. Choosing the Hospital
Ideally you would choose a hospital on the quality of the psychiatric care the patient is likely to receive. However, in recent years the overall quality of hospital care has been eroded and differences between hospitals equalized by costs, competitive forces and insurance limitations. In general, you try to get the patient to a safe place.
Generally, it is a good idea to become familiar with the choices in your area, through talking with other therapists and with people who have been there as visitors or patients. When possible, site visits help develop an impression of a facility and its staff.
If you are forced to commit a patient involuntarily by calling the police, place of hospitalization will be determined by catchment area, and you will have no choice in the matter. However, family members can sometimes arrange for a transfer if they are dissatisfied with the care in the initial hospital.
11b. Preparing a Patient for the Hospital
Usually the patient goes to the hospital emergency room, if possible, accompanied by a friend or family member. Alternatively, you may take the person, or have someone else take him/her, or call the police emergency number for an ambulance to take him/her.
At the ER, the patient will tell his/her problem to the receptionist, who will call for a psychiatrist or intake worker to speak with him/her.
Patients should expect to provide a lot of information in a very short time. Part of the information that the patient offers should be that he/she has been in treatment with you. You should get written consent from the patient to talk with hospital staff.
Some attention should be paid to the patient’s feelings and expectations about the hospital experience, to help reduce anxiety and deal with misconceptions. With some patients – and some hospitals – you may need to say that the hospitalization is necessary.
Patients should appreciate the purposes of hospitalization:
- to be in a safe place until the suicidal feelings fade a bit
- to find a medication that can help and determine the right dosage
- possibly, to deal with some personal issues intensively
- to recognize that other people have similar issues
You may discuss having visitors, and the possibility of your having sessions or a visit while he/she is there.
11c. Process of Hospitalization
There are various ways that you can send a patient to a hospital.
If you have admitting privileges, you may make the arrangements directly. If you have a prior arrangement with the psychiatrists at a hospital or someone who has admitting priviledges, you may be able to make use of that relationship to get a patient in.
You can send a patient to the emergency room at a hospital, where he/she can explain his/her problem and obtain a psychiatric examination. If a patient is severely enough depressed to require hospitalization, this method involves some risk. It may be better to send the patient with someone else, such as a friend or relative.
If the patient is resistant to going, you may need to have someone else take him/her to the emergency room.
If the patient is clearly dangerous to him/herself and unwilling to go to the hospital, you may feel forced to arrange for involuntary commitment. This may include calling the police by dialing 911, and asking them to arrange for commitment.
11d. Coordinating Treatment
It can be helpful to be in touch with the hospital beforehand, to make sure that there is an available bed in the unit.
Calling the unit once the patient is there can be helpful to hospital staff. If you don’t call, a good hospital will typically call you. A therapist can provide relevant information that the patient might not volunteer and that might not be part of usual intake data. Therapist information may be more reliable than patient information.
Sometimes hospital staff will be very happy to have an outside therapist available, so they can release the patient into your care quickly. You may have to be very clear that you are not able to take responsibility for the patient, that you only provide treatment.
Sometimes, when you believe that your work with the patient is not being helpful, you may want to use the hospital stay as an opportunity to discontinue treatment with less rejection trauma to the patient. It is the hospital’s responsibility to come up with an appropriate discharge plan. If you indicate to hospital staff that you do not have the resources to deal with this patient and the kind of risk that he/she presents, they might not like you for it, but they will have to come with another plan.
Follows Section 10 on Map 1B. Coordinates with New Patient Section 16
Commonly a long-term care option for severely depressed individuals, possibly as a sequel to hospitalization.