14. DECISION ABOUT PRIMARY OUTPATIENT TREATMENT
- This section follows Section 20 on Map 5 and coordinates with Section 19 on Map 5. It leads to Section 15, Section 16, Section 17, Section 18 or Section 22, depending on patient needs.
At this point, a decision must be made about the primary type of outpatient treatment to be offered. This decision will be based on a number of factors, and it may have to be revised as you learn more about your patient. Decisions made at this time also may not be optimal in the long run, because the person’s needs may change as time passes and work is done on sobriety and other psychological issues.
It should be noted that people in the contemplation, preparation or action stages of change [ Section 47 ] are likely to be involved in treatment at this point. However, a person in the precontemplation stage will probably not be interested in pursuing any discussion of alcohol treatment, and the treatment may have to be limited to acceptable topics. Some work can still be done relative to the patient’s drinking as new information comes up in the therapy or in adjunctive care consultations.
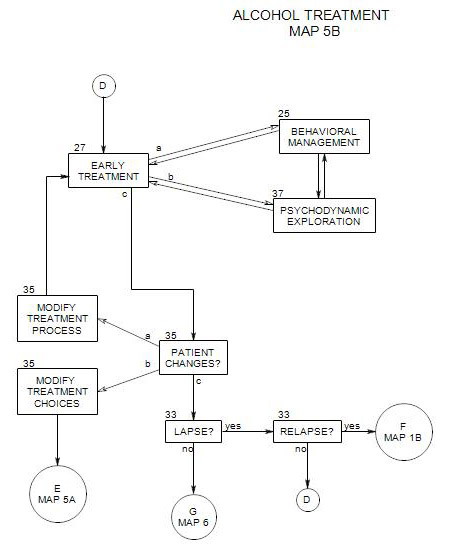
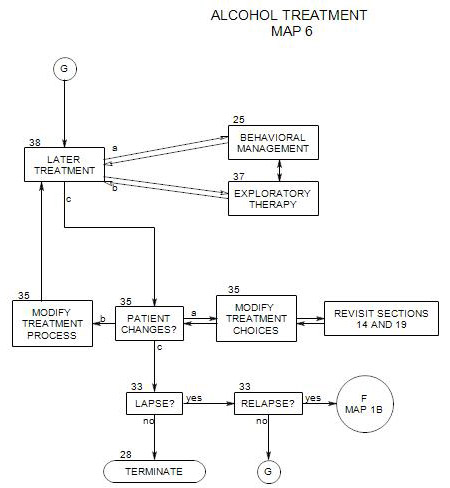
An important distinction is the one between behavioral management and insight. Early on in the treatment of alcoholic patients, it is especially important to help them take control of their drinking behavior, and treatment choice should work toward strengthening that aspect of treatment. Later, once behavioral control is more stable, exploration of underlying motives and interpersonal relationships may be helpful both in avoiding relapse and in dealing with other psychological issues that affect the patient.
This section considers
- The usual choices for form of treatment – individual therapy, group therapy, couple work, family therapy and self-help groups – and their relative advantages and disadvantages
- Making the choice of primary treatment modality
14a. The Choices, Their Advantages and Disadvantages
INDIVIDUAL PSYCHOTHERAPY
This is the most common primary form of treatment in outpatient private practice settings. The rest of this book is written from this perspective.
There are a variety reasons that individual psychotherapy may be the treatment of choice for a patient. Many have to do with availability or flexibility:
- It is widely available, and alternatives may not be.
- It may be the only approach that a patient will agree to.
- It allows great flexibility in including other forms of treatment as adjunctive and tying them together with the primary modality.
- It is flexible in terms of time of sessions and length of sessions.
- It allows fluid movement among issues – especially between alcohol misuse and other psychological issues.
- It offers flexibility in working with behavioral goals early in treatment and switching to primarily exploratory therapy later on.
- The degree of emphasis on behavior management versus exploration of underlying motives and conflicts can be varied at any point in treatment, according to the patient’s needs and the abilities of patient and therapist to work with the different approaches
- It has the potential for a deeper level of exploration than other forms of treatment, because of the ability of the therapist to make specific connections between the patient’s behavior and his/her thoughts and feelings.
- The therapist can easily explore the patient’s individual background and personal history as an aid to understanding current expectations and pressures and the likelihood of future pressures.
There are also disadvantages: to individual psychotherapy:
- It is easier for a patient to hide the fact of his/her drinking than in group or family work.
- It may be difficult for a therapist to confront a patient who is drinking and lying about it, even when the therapist is aware of the truth.
- A patient’s insurance may not pay for individual treatment for alcohol misuse.
GROUP THERAPY OR COUNSELING [described in Section 18 ] is often the most effective form of treatment early in recovery, and typically the primary form of treatment in inpatient settings and partial hospitals.
Relate to stages of change, support for an intervention, dealing with precontemplation
For this decision the most appropriate group is probably an early sobriety group or a socialization group. A therapy group which doesn’t have alcohol or addiction as a major focus may miss the most important treatment issues for an alcoholic patient.
Advantages to group psychotherapy [especially an alcohol treatment group] include the following:
- The patient can be confronted by other alcoholics in recovery who have their own issues and problems. The group process is very powerful. It is difficult to maintain denial in the face of confrontation by one’s peers, who are all facing common issues.
- The patient may come to identify with the recovery of other people in the group, increasing motivation for his/her own work.
- Each of the other group members is potentially a resource and a source of support, and group members often rely on each other outside of the treatment setting.
- Group therapy may be the only form of treatment an insurance company will pay for, especially if the patient’s primary diagnosis is drug or alcohol related.
There are also disadvantages to group therapy, including:
- Compared to individual psychotherapy, the work may be less intense.
- It is not tailored to the needs of any particular person, although at times it may fit them well.
- A quiet person could get lost in a group.
- The type of group may or may not match patient’s place in recovery, and will be more or less appropriate according to the degree of match.
- The group may or may not be focused on psychotherapy.
- The group may or may not be focused on drug and alcohol treatment.
COUPLE THERAPY
Although you can work with an identified patient and any other person as a couple, in practice it is usually limited to two people who are of the same generation and in an intimate –though not necessarily sexual – relationship. [Couple therapy is discussed in Section 17.]
Typically, what happens to one member of a couple affects the other, and an alcoholic’s partner can be participating in his/her problem in many ways. The partner may be reacting to the patient’s issues and need help in separating from them; and/or the partner may be contributing to the patient’s drinking behavior or psychological difficulties either directly or indirectly.
The partner may enable the patient’s drinking behavior in many ways, by providing access to alcohol, excusing the drinking behavior, resolving negative consequences or protecting the patient from experiencing them, taking over when the patient fails to carry out responsibilities, and so on. The partner may become codependent by abandoning his/her own best interests in order to maintain the relationship and protect the alcoholic patient. The partner may also have his/her own alcohol issues that need to be addressed.
There are several advantages to couple therapy, including
- You can get ongoing, intimate information about the patient that you might not be able to obtain in any other way.
- The patient’s partner knows him/her best and often will be an active participant in the treatment.
- The partner is likely to be an active participant in the patient’s drinking, in one way or another, through shared drinking, enabling the patient to continue drinking, reacting negatively and destructively or being codependent with the patient. In couple therapy the two people can be treated together, and their interpersonal system addressed.
- Sometimes, as the identified patient recovers, the partner’s pathology becomes more obvious. When this happens, couple work can help identify the newly obvious issues and offer you the opportunity to modify treatment to deal with them.
- If the partner is not engaged in the therapeutic process, his/her issues could go unnoticed or unaddressed and potentially undermine treatment with the identified patient.
Disadvantages to couple work can include the following:
- The patient’s partner is not an unbiased observer, may have his/her own pathology, and often has an ax to grind relative to the patient’s treatment. This could be distracting or destructive.
- The patient’s primary issues may not involve the partner, and couple work may distract from needed individual work.
FAMILY THERAPY
This [See Section 22 for a description of family therapy.] may be especially helpful in times of crisis or later on in recovery. Here the term “family” is used broadly, to include unrelated individuals who are significant to the patient. It may also be narrowed, to include only the immediate family, and to include younger and older generations as needed. Family therapy also encompasses marital treatment [ Section 17 ]. Commonly the marital couple is the center of the family, and they may need to be dealt with before bringing in the rest of the family.
Advantages of family therapy include
- Flexibility: it can include various combinations of individual, marital or couple, or whole-family treatment.
- Efficiency: If several family members are heavy drinkers, then it may pay to address that and related issues as a group, and enlist the entire family in dealing with common problems.
- Any change in an alcoholic patient will have an effect on other family members, who may, consciously or unconsciously, resist it. Family therapy can address those resistances directly, with an impact on the patient’s individual therapy.
- At the same time, family therapy can explore the effects of the patient’s alcoholism on the family and the alcoholic’s role as identified patient.
- Relationships, expectations and conflicts within the patient’s family may be contributing to the patient’s intrapsychic issues and/or drinking behavior. If the family dynamics can be altered, then some of the pressure to drink can be reduced. Family therapy can address these problems directly.
- Commonly drinking is related to various kinds of psychopathology, and family therapy may help uncover the individual pathology of other family members, who can then be referred for their own treatment.
- When change in family dynamics is indicated, it can be more effective for a therapist to work directly with family members than to try to work through the patient.
There are also disadvantages to family treatment, including
- Family therapy is stressful. Early on, you are training the patient to stay sober in the face of small increments of anxiety. A family session in itself could provoke a relapse.
- A patient may not have a family or significant others.
- The work may focus on the needs of others in the family, and be less intensely directed to the issues of the identified alcoholic patient.
- Some pivotal family members may refuse to participate, or find other ways to undermine the treatment.
Family therapy may be the modality of choice if
- family conflicts or relationship problems are contributing to the substance abuse of the identified patient.
- family members are enabling the alcoholic patient to drink by not speaking up or otherwise confronting him/her.
- other family members have been adversely affected by the alcoholic patient.
SELF-HELP GROUP
These groups are typically composed of other people facing similar issues to the patient’s, especially in their alcohol involvement [For more, see Section16.]
Advantages of a self-help group as the primary form of treatment include
- Groups provide a variety of supports that help a person deal with the urge to drink, including regular availability, non-judgmental attitude, respect for individual differences among members, guidelines for self-management, and sponsor involvement.
- It may be the only form of help that some people can accept, because of a perceived stigma attached to psychotherapy or counseling, a fear of the therapist’s power, a fear of being found out to be crazy, etc..
- Staying sober may be all that a person feels he/she can manage, for a while, and he/she may see the group as the only effective treatment form.
- There may be considerations of cost and availability that make such a group the preferred form of primary support.
- Identification with other group members can help a person recognize his/her own issues.
Disadvantages: may include the following:
- Attendance is voluntary and not monitored. A person’s attendance may be consistent or spotty, with little outside pressure to continue.
- Some patients refuse to go to meetings, because of fear of the group process, aversion to what they see as a religious tone, or other reasons.
- Making the referral can be difficult. See Section 16 for some suggestions here.
- A person may have difficulty with a particular group and be reluctant or unable to try others.
- Self-help groups typically don’t work at the same psychological level as therapist-managed forms of treatment.
- AA and most other self-help groups have abstinence as their goal, and a person who wishes to continue drinking can feel out-of-place.
14b. Making the Choice
Whether a patient comes to you for the first time or is returning after more intensive treatment, this is a good opportunity to explore the patient’s needs, financial resources, etc., as a basis for choosing a primary form of outpatient treatment.
The first question to ask at this point is “Who decides?” Has the patient already chosen a form of treatment by coming to a particular therapist? Are patient and therapist assuming that the therapist will decide, or will they make the choice together after reviewing the patient’s needs and the options available for meeting them?
t is important to match the treatment to the patient’s ability to benefit from it. This is a good time to make a formal treatment plan, including short- and long-term goals, patient strengths and limitations, available resources, and any likely adjunctive care [see Section 19 ]. Some of these issues will be considered again in the section on early ongoing treatment.
For example, you might recommend both group and individual therapy or individual therapy and self-help group membership. If the patient has not been through a chemical education series (e.g.: during rehab) then that could also be an important part of treatment.
Following are some issues that can affect treatment effectiveness. There is no inherent order to them, because the priorities are likely to differ from one patient to another. There is also no formula for combining the information from the different considerations into a single set of choices. Patient and therapist work together to make the best choices they can, with the possibility that different decisions may need to be made at any time in the process of therapy.
PATIENT STAGE OF CHANGE
People in different stages of change [ Section 40 ] need different approaches.
When a person is in the precontemplation or contemplation stage, too much pressure for change may be resisted. In these stages, group therapy, with its intense focus and social pressure for sobriety, may not be a good choice. A patient might refuse to participate, and withdraw from other forms of treatment as well. For these people, individual, couple and family therapy offer a more diffuse focus and the opportunity to look at the person’s drinking as it becomes relevant. Then it can be examined in a larger context and at a pace that the person may find easier to respond to. By contrast, people in the preparation or action stages may welcome a treatment modality, such as a self-help group, that provides greater pressure toward abstinence.
AVAILABLE TREATMENT MODALITIES
Choices must be made from among the options that are available, and some searching may be necessary to find appropriate matches to patient needs. The issues here include
- whether the services that the patient needs are available at all.
- whether a given therapist has time available to see the patient, and whether there will be a wait before treatment can begin.
- how far the patient will have to travel and the form of transportation the patient will use to get to therapy. Whether services are available at that times that the patient is available.
- the personal qualities and reputation of therapist, as well as therapist specialties and weaknesses or limitations.
- the focus of treatment and with each treatment option whether it addresses the patient’s primary needs adequately.
- in the case of group work, the quality and focus of available groups and the patient’s prior experiences with groups.
- the patient’s other commitments and responsibilities, such as work, medical treatment and child care.
PATIENT RELATIONSHIP WITH ALCOHOL AND ALCOHOL TREATMENT
It is also useful to know when and how the patient drinks or drank – what functions it supported, what needs it met, and so on.
For example, a social or party drinker might do well in group therapy, where there is contact with many people, and they are working on achieving and maintaining sobriety. A social phobic person might do better in individual or couple work, where group issues won’t be distracting.
PATIENT’S TREATMENT PREFERENCES OR FEARS
It can be helpful to discuss the available treatment modalities with a patient, to discover his/her issues relating to each. A person may be
- afraid of groups and a group’s influence; or just shy.
- unwilling to raise certain issues for discussion in couple therapy but able to work on them individually.
- insecure in his/her status and role in his/her family, and unwilling to have family members participate in treatment.
- unable to convince a spouse or family to participate.
- unconvinced that individual therapy can be of help but willing to attend self-help meetings or couple therapy.
TREATMENT HISTORY
In evaluating various treatment modalities, it helps to know what the patient’s prior experiences have been. They provide a perspective from which to discuss patient expectations, attitudes and remaining treatment needs. Some forms of therapy may seem natural and familiar; others may be unacceptable because of expectations or prior history. If a particular modality has been effective in the past, it may be a good choice for the current episode. If the patient has a long history of ineffective treatments, something new may be in order.
The patient’s immediately previous alcohol treatment may also have an impact on the kinds of treatment that will be most helpful, because of the kind of help that was received and its effectiveness.
PATIENT’S OTHER PSYCHOLOGICAL DIAGNOSES
Many alcoholic patients have co-occurring psychological conditions, which can either be a consequence of drinking or which the patient tried in the past to manage with alcohol. You will most likely need to treat both alcohol misuse and some psychological disorder at the same time.
The more severe the patient’s psychological issues, generally the more services may be needed, either from you or other professionals or organizations. Different services need to be coordinated in order to be maximally effective. If the patient’s needs are too diverse and serious, referral to a multidisciplinary treatment facility may be the optimum choice.
COSTS
A patient must be able to afford therapy or he/she is likely to
- refuse to go.
- drop out, or
- neglect other aspects of living in order to pay for treatment.
A therapist can’t decide for a patient about the relative costs of various treatment options and the patient’s ability to pay, but it can be helpful to discuss the issues. The discussion may help the patient re-examine and formulate financial issues, or obtain appropriate insurance. It may also demonstrate that sensitive areas of living can be safely discussed in treatment.
Considerations include the following:
- Typically individual therapy is more expensive than group. AA and many other self-help groups are free.
- Different therapists charge different fees, and the differences matter to many patients. Some therapists may not accept the patient’s insurance or participate in the patient’s managed care panel. If there are clinics nearby, they may offer free or low fee therapy.
- Once you report that a patient has an alcohol problem, some insurance companies may only pay for short-term group therapy, regardless of patient need. They may also specify the qualifications of the treating person or facility. If you decide to treat an alcoholic patient individually, you and your patient must decide how to deal with insurance.
AVAILABLE SUPPORT FROM FAMILY, FRIENDS AND COMMUNITY
The person’s family and social environment should be examined with the patient, to determine whether they provide support for continued sobriety or pressure to return to drinking. If the latter, then that pressure needs to be countered in some way, to help the recovery process. You can ask who in the family is likely to be supportive, and who will probably interfere with treatment; who provides a model for drinking or remaining sober; and how to include other family members and help them be supportive. See Section 21 for more on this.
If there are issues with the patient’s neighborhood, peer group or larger environment, these should be addressed as well.
THE CHOICE OF ADJUNCTIVE CARE
Your decision about the primary form of treatment should also be made in conjunction with your choice of adjunctive care for the patient [ Section 19 , and may be influenced by the latter.
For example, individual psychotherapy might coordinate well with self-help group participation for some people, and each modality could support and feed into the other. Medications could be helpful in dealing with some issues that the patient has used alcohol to manage, relieving constraints on the types of therapy that can be effective.
When two or more modalities are used in concert, any one of them could begin as primary, with the others as adjunctive. This relative importance could shift in the course of treatment.