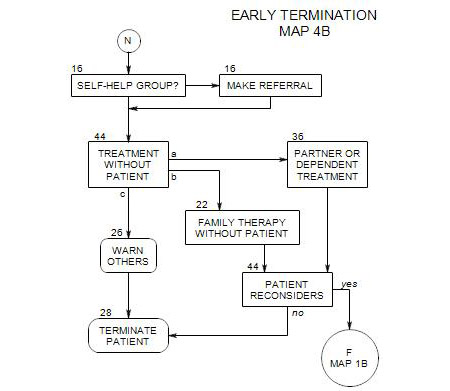
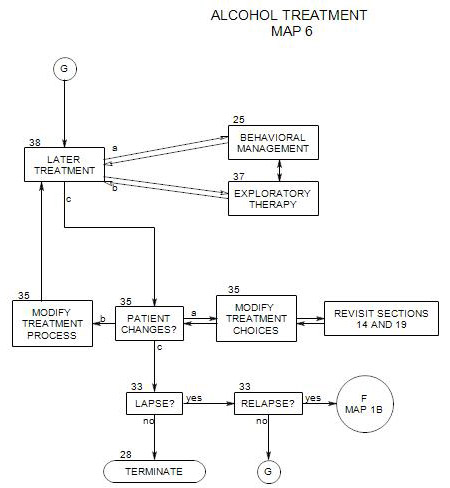
28. Termination
Endings are as important as beginnings, and need to be given the same level of attention and respect. The way a person leaves treatment will have a major impact on the attitudes and thoughts he/she carries forward.
Termination can come about in a variety of ways and at virtually any point in treatment.
- It may be a planned part of treatment
- The patient may give prior notice of intent to leave
- The patient may simply stop coming, without prior notice
- The therapist may be forced to terminate treatment
Every termination should be documented as to reasons, issues and the process followed. Documentation can facilitate picking up treatment if the patient returns at a later date, ease a possible referral to another therapist, or provide information to adjunctive providers.
There are some special dangers at this point. A patient may leave treatment as a prelude to drinking again, and that in turn can lead to serious risks for the patient and/or others around him or her. The way that the person terminates may have an impact on his/her attitude toward you and toward future psychotherapy, and the effectiveness of all that has gone before. Patients talk to friends, family and other professionals, so your reputation and future referrals can be impacted by the attitude that a patient leaves with. For a discussion of other dangers, see Section 6.
It may be necessary to inform others of the termination [ Section 26 ], if it appears that they are at risk.
28a. Planned Termination
Ideally, termination is planned as a consequence of having completed work on the person’s alcohol issues and any psychological issues as well – at least for now. It is a natural outgrowth of the work you have done together.
A planned termination should be a joint construction, with flexibility of the termination schedule. It can take anywhere from a single session to several months to conclude treatment, and a formal date may or may not be part of the plan.
The termination process should include most or all of the following components, if possible:
- Review and evaluate the treatment to date: accomplishments, changes of symptoms, changes in behavior and thinking, issues remaining, etc.
- Discuss the termination process itself: what to expect and how it could go. Discuss the patient’s reactions to terminating.
- Decide about whether to taper sessions or not, and if so, by what formula.
- Consider further work that may be ahead for the patient.
- Arrange for continuation of whatever adjunctive or other care is still needed.
- Decide whether to refer the patient for additional treatment in another modality or with another therapist.
- Decide whether to terminate for a while and plan to resume a new course of treatment at a later date. Discuss possible occasions for the patient’s return and reasons the patient might need to contact the therapist.
Termination also involves dealing with endings and losses, which can bring a resurgence of dependency issues, separation anxiety and other psychological issues, and a renewed possibility of relapse. These concerns are discussed by Rockland [161-172].
Termination Criteria
There are a variety of criteria for the end of treatment, depending on the treatment goals. With patients who are misusing alcohol, there may be two different sets of goals: one set for alcohol treatment and another for therapy of the person’s psychological issues. Alternatively, treatment goals will have changed from a primary focus on alcohol treatment to a greater emphasis on other psychological issues, and termination may be more about the patient’s psychological changes than alcohol treatment.
However, not only may the goals of recovery and the goals of psychotherapy differ, the patient may be working with a counselor for the recovery part and a different therapist for psychotherapy; in this case, there would likely be two termination processes that differ with regard to timing and issues.
If the therapeutic contract is limited to alcohol recovery, termination criteria typically have more to do with behavioral management issues than psychological awareness. The criteria generally include
- The patient is stabilized in abstinence. As a rule of thumb, there should be at least 6-8 months of total abstinence before termination of alcohol treatment is considered. Along with that, it is essential for the patient to have developed, and consistently practiced, his/her program of recovery for several months before the termination phase is begun.
- The program of recovery should include active involvement in AA or another a self-help group, with regular attendance, participation, and a sponsor and home group.
- The patient’s probability of relapse is small under normal circumstances, and reduced under conditions of high stress. This means that the patient has tools for dealing with relapse temptations: identification and avoidance of triggers, etc.
- Environmental and other psychological pressures to drink are known and have been reduced. Pressures that can’t be relieved are avoided whenever possible.
- The patient has social supports for sobriety in the form of family and friends
- Other lifestyle changes have been made to provide ongoing support for sobriety
If the patient has moved on to emphasize other major psychological issues, then termination depends on the nature of the other issues or diagnoses and the type of therapy used in treatment. Generally the conditions for termination include:
- The patient’s treatment goals have been met
- The patient’s initial symptoms have been reduced or eliminated. Gains have been consolidated.
- The patient is able to pursue his/her personal goals without professional help.
- The patient is better able to adapt to his/her world and cope with adversity.
- In addition, if treatment has been more cognitive, then a condition may be that the patient has learned techniques for managing disruptive emotions and behavior.
- If the treatment has been more psychodynamic, then conditions for termination may include a reduction in the intensity and disruptiveness of basic conflicts, reduction in the perfectionism and fantasies of childhood, increased self awareness, self soothing, and self control.
28b. Patient Gives Notice of Termination
If your patient warns you that s/he won’t be returning, that is your cue to begin either a re-evaluation of treatment or a termination.
If the announcement is tentative or questioning, then you can examine the issues of Part 28a from the perspective of determining whether termination is appropriate at this time. If the announcement seems firm, you can agree and then suggest a need to examine the arrangements in order to have an effective ending. If the patient agrees, it becomes an opportunity to re-evaluate the treatment and treatment goals.
If there is enough advance notice, you can begin to deal with the patient’s issues immediately. However, sometimes a patient will make the announcement as s/he is walking out the door at the end of a session [“Oh, by the way, -“]. That should be your cue to press for another session, to end properly, to understand fully the patient’s need for a termination at this time and this way, to evaluate the treatment and changes the patient has made, and to plan together the patient’s next steps.
A patient may cite one or more motives for termination, including
- Circumstances have changed: the patient was in an accident that requires extended physical recovery, his/her job requirements are forcing a change in schedule or additional work time, family demands have changed, etc.
- Practical issues interfere: the patient can no longer afford your fee, he/she is moving away, etc.
- Belief that he/she has to stop for some reason, such as insurance limitations
- Belief that treatment goals have been met – [if the crisis is over]
- Loss of motivation to continue because of other pressing issues leading to new opportunities and responsibilities, such as getting married, the birth of a child or a promotion at work
- Belief that the terms of treatment [fee, frequency of sessions, times of sessions, etc.] are fixed, and he/she must accept them or leave.
Whatever the motives cited, they should be examined as part of the termination process. Patients may give what they consider reasonable and socially acceptable motives as cover for less desirable ones.
In the case of termination, you should also include a record of the termination discussion and any decision that was made.
28c. Patient Leaves Without Prior Notice
This case amounts to an unpredicted and unexpected [temporary or permanent] disruption of treatment. It could happen at any time, for any one of a variety of reasons. The crucial piece is that you don’t know the reasons a person has left treatment.
It may have been done because of a misunderstanding that you can clarify in a follow-up; or the patient may have a legitimate complaint about you or the treatment that can be addressed and resolved. It could also be that the patient was overwhelmed by an unexpected event and moved on without notifying you. Patients often don’t think to call their therapists when they are being rushed to a hospital. Patients who suicide may not call first. The problem is that you may not learn what happened until you contact the patient and ask the question.
There are many ways to reach people today – telephone, email, regular mail, texting, etc. If you are successful, you can explain the need for another session, continuation of treatment, or further planning of ways to deal with the patient’s remaining issues. If you can’t reach your patient directly, you may try an indirect approach, possibly calling a relative, if that wouldn’t be considered a breach of confidence.
If the patient can be reached and agrees to come in for “one more session”, then move to the process as described in Part 28b above
You may also decide to inform others of the termination [ Section 26 ], if you think that the dangers warrant that action. Dangers: This depends on whether you believe that leaving treatment is a prelude to drinking again, and that in turn leads to serious risks for your patient and/or others around him or her. For a discussion of dangers, see Section 6.
In the case of abrupt termination, you should also include a record of the termination process: how the patient left and any attempts you made to contact him/her. Especially when you are unable to reach the patient, it is important to have a record of the circumstances under which he/she left, the issues being discussed, attempts you made to reach him/her, and so on.
28d. Therapist Forces Termination
There may be circumstances under which it is necessary for a therapist to end treatment before the work is finished.
- It may be a part of the process of referring the patient out to a self-help context or another therapist. This can be handled as a planned termination, as in Part 28a above.
- It may be a reaction to a patient’s having a relapse and needing to go for inpatient treatment before continuing. How it is handled depends on the circumstances of the relapse, the amount of lead time before the patient goes into treatment, and the ability of the patient to come to sessions and work on preparation before going. If the therapist participates in forcing the patient into unwanted inpatient treatment, the patient may not return to therapy on release from the hospital or treatment center.
- A therapist may refuse to continue treating a patient who refuses to deal with an alcohol problem or other addiction,. Without a commitment to treatment or , further work is unlikely to have any real effect.