SECTIONS: 5 | 8 | 16 | 19 | 21 | 22 | 24 | 25 | 39 | 44 | 46 | 47 | 48
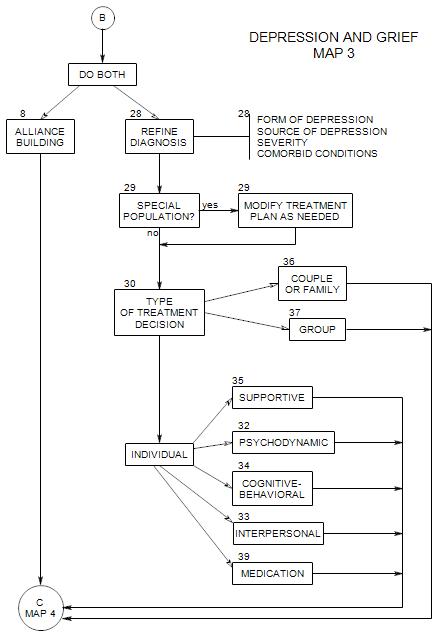
SECTIONS: 8 | 28 | 29 | 30 | 32 | 33 | 34 | 35 | 36 | 37 | 39
-
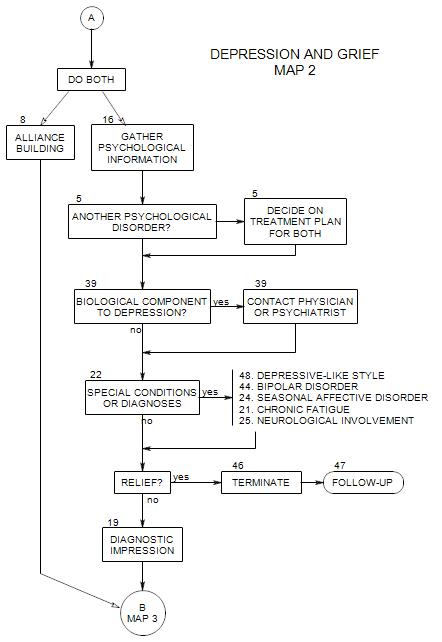
Follows Section 19; top of Map 3
We have now ruled out or accounted for some major possible sources of depression, and are left with a patient in a depressed state and in need of further diagnosis and treatment.
At this point, we are putting together information we have already gathered about the patient’s depression, and possibly gathering more.
Because our primary interest is treatment, we will focus on diagnostic information that affects treatment choices. Distinctions made by the DSM may or may not affect our focus or way of operating with a given patient.
In addition, the person may or may not have flagrant symptoms, the problem may or may not have a biological component, and the depression may or may not be responsive to medication.
28a. Episodic VS. Longstanding
FIRST EPISODE
If this is the patient’s first depressive episode, you will want to inquire into the circumstances when the depression began, to explore…
- the amount of stress the patient was experiencing
- the kind of stress
- the patient’s ways of coping, and why they failed
- possible secondary gain from the depression
MULTIPLE EPISODES
If there were other depressive episodes, we want to know how they were similar and different from the present one, to look for patterns.
If there have been other depressive episodes, we will also want to know about any periods of mania or hypomania, and also about periods of euthymia. The distinction between bipolar disorder and simple depression affects the choice of medication. You also want to understand manic periods, and to be prepared in case the patient goes into a manic state. Manic patients often are not compliant regarding their medication.
Part of the psychotherapy may involve helping the patient adjust to the loss of mood swings as a result of medication. Patients may regret the loss of the manic phase of the illness, and stop taking medication in order to experience that phase again. Also, some people in a manic phase may take actions that have long-term negative consequences [e.g.: ]
LONGSTANDING DEPRESSION
If the patient’s depression is longstanding, you may not be able to identify any precipitants. In terms of treatment, you are more likely to look for dynamic issues rather than environmental pressures. You may expect more resistance to change because the patient – and the patient’s family – may have adapted to the patient’s depression. The patient may also be deriving some secondary gain from his/her illness.
It is also possible that there was a chronic predisposition that was environmentally triggered, either because of increased stress or because the precipitating event raised old, unresolved issues.
28b. Severity of Depression
You need to know how deep the patient’s depression is, not only relative to the issues of medication and hospitalization, but also in order to plan the types of interventions that are likely to be helpful. A mildly depressed patient is more likely to be an active participant in his/her own treatment. A more severely depressed person may be more passive. With a more severely depressed person, interventions that rely on a patient’s consistency, reliability, insight, etc. may fail because the patient is confused or discouraged. This can include medication compliance.
28c. Psychological or Biological Origins
It is often not clear whether a particular depression is [a] primarily biological, with intrapsychic and interpersonal experiences following from the patient’s neurological or biological state, or [b] primarily cognitive or emotional, with biological changes occurring as a consequence of the person’s mood, thinking, or way of operating in the world.
28d. Triggers
When the person’s depression is a first time, or if it is episodic but the timing is irregular, you may be able to find some event, thought or experience that initiates the episode. This can be explored for psychological meaning. It is possible that a thorough exploration can lead to re-framing and reduction in the severity of the depression.
When the depression seems more biological, it may not be possible to identify a trigger for an episode. In this case, the person may not be able to get at the root sources except by biological means; medication, exercise, and living through the episode.
28a. Formal Diagnoses
In terms of the ICD or DSM, we are now considering primary diagnoses in the mood disorder range, such as the following:
- major depression [296.2, 296.3] severe depression of any length.
- dysthymia [300.4] relatively mild depression but longstanding
- depressive disorder [311]
- bipolar I [296.0, 296.4, 296.6, 296.5, 296.7] Periods of mania.
- bipolar II [296.89] Periods of hypomania
- bipolar [296.80]
- cyclothymia [301.13] Mood swings but less severe.
For a thorough statement of each of these diagnostic categories, see DSM IV