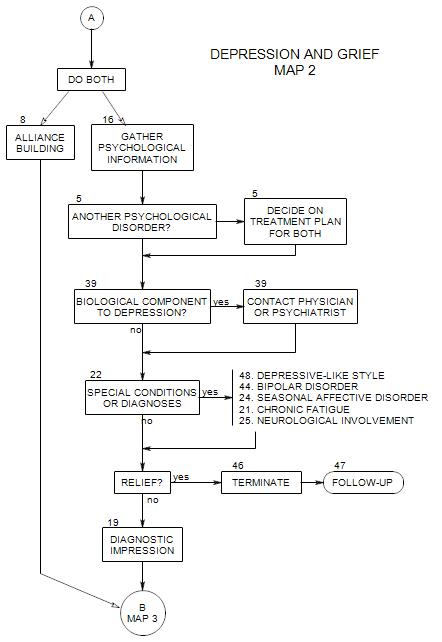
SECTIONS: 5 | 8 | 16 | 19 | 21 | 22 | 24 | 25 | 39 | 44 | 46 | 47 | 48
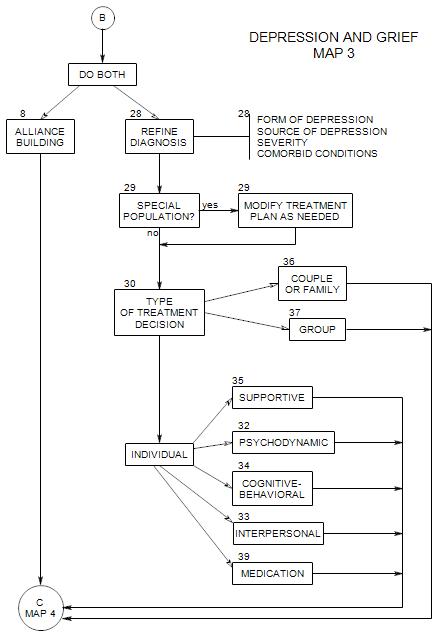
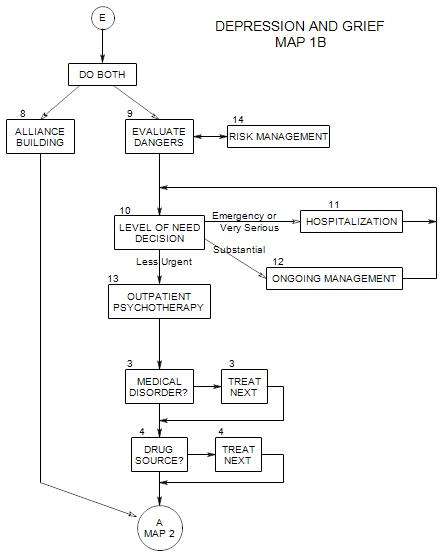
SECTIONS: 8 | 28 | 29 | 30 | 32 | 33 | 34 | 35 | 36 | 37 | 39
-
Follows Section 39 on Map 2
At this point you may be able either to identify a specific reason or cause of the person’s mood problem, or on the other hand, eliminate some possibly confusing issues.
Watch for
- Post-Traumatic Stress Reaction [PTSD]
- Seasonal Affective Disorder [SAD]
- Neurological complications
- A depressive style
22a. Symptoms of Post-Traumatic Stress
Usually considered an anxiety disorder, post-traumatic stress can also lead to a reactive depression, as the patient becomes discouraged about re-experiencing the same symptoms, not getting better, being different from other people, and possibly having caused the trauma.
In addition to depressive-like symptoms or depression, the patient…
- is reacting to a stressor that is more extreme than most people ordinarily experience: flood, airplane crash, being held hostage, etc., either experienced personally or witnessed.
- continually re-experiences the event, through dreams, fantasies, over-reacting to other events, flashbacks, etc.
- consistently avoids associations to the event, either consciously or unconsciously. This can constrict his/her thinking, emotional range, and ability to move about.
Treatment is considered in Anxiety Section 9.
22b. Identification of Seasonal Affective Disorder
Seasonal Affective Disorder consists in a variability in mood (and biological rhythms) as a function of changes in daylight.
WINTER DEPRESSION
In the autumn, the person becomes mildly to moderately depressed and may…
- become sad, anxious, irritable, socially withdrawn
- have difficulty concentrating and taking initiative
- feel lethargic
- sleep too long
- crave carbohydrates and gain weight
- use stimulants [coffee, chocolate] or alcohol, in an attempt to treat the depression
Commonly, symptoms worsen as the days shorten, with January and February being worst.
With the coming of spring, the person may [or may not] develop a hypomanic phase, with
- increased sense of well-being
- improved creativity
- decreased need for sleep
- reduced appetite and loss of weight gained during the winter
- impatience and irritability
In some cases, this can become an actual manic phase.
Patients with SUMMER DEPRESSIONS tend to follow a more standard depressive pattern, with insomnia, loss of appetite, and loss of weight.
See Section 24. Seasonal affective disorder for treatment.
22c. Identification of Neurological Issues
Any complaint in which a neurological condition could be a contributor to the patient’s depression. Signs of neurological involvement can include…
- memory problem, recent onset
- recent loss of ability to concentrate
- history of possible head injury
- cognitive impairment
- early stages of dementia [see Appendix ]
For treatment implications, see Section 25. Neurological Involvement.
22d. Identification of Depressive-like Style
A person who lives under constant stress and is unable to be free about self-expression may develop a depressive-like style that reflects a defensive way of relating to the world rather than actual depression.
Someone like this is unlikely to appear for therapy for depression but could come in for another condition. The best early information comes from asking about depressive symptoms directly.