SECTIONS: 5 | 8 | 16 | 19 | 21 | 22 | 24 | 25 | 39 | 44 | 46 | 47 | 48
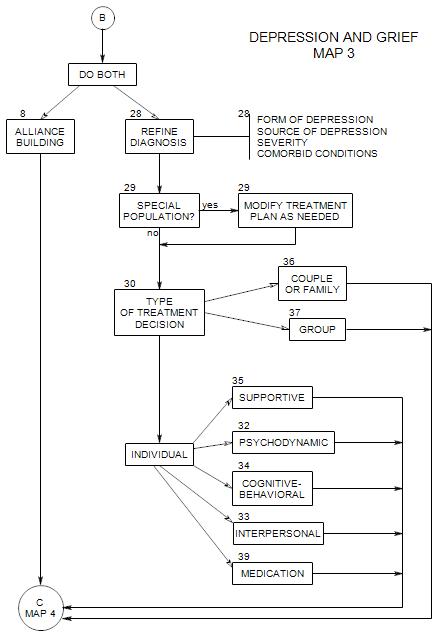
SECTIONS: 8 | 28 | 29 | 30 | 32 | 33 | 34 | 35 | 36 | 37 | 39
-
Follows Section 30 on Map 3
32a. Psychodynamic Understanding of Depression
A psychoanalytic approach treats depression as a personality issue, not primarily as a mood-state. The depressed person’s issues are longstanding, and while some temporary relief can be obtained through symptom-focused treatment, it can’t be expected to last. In the long run, temporary “fixes” can discourage patients, when the depression returns.
Depressed patients can be identified by characteristics that operate even when they are not in a depressed mood.
Psychoanalytic work assumes that much of the thinking that leads to the patient’s depression is out of the patient’s awareness; otherwise the patient would have made necessary changes on his/her own.
Specific issues and functions that need to be addressed can, and often do, include the following:
Structural Issues: [1] excessively strong and punitive superego, leading to frustration at not being able to meet one’s own standards and a sense of being bad and guilty; [2] a grandiose ego ideal that the actual self is unable to live up to, leading to a sense of being inadequate; [3]. Conflicts between superego limits and id wishes
Genetic Issues: [1] history of early separation and loss that was out of the patient’s control, leading to chronic high drive state, sense of worthlessness, idealization of the lost person, rage at an abandoning person, sense of helplessness and hopelessness, fear of driving away any new object, etc., much of which is unconscious but still affecting the person. [2] depressed parent and/or other family members [3] family that discouraged grieving and the processing of losses
Ego Deficits: poor reality testing
Defenses: [1] Most powerful is introjection, often of the negative qualities of an important person from the patient’s past; [2] turning against the self, eg: feeling that he/she deserved to be abandoned or rejected, or perhaps caused it; [3] idealization of others, which leads to feeling more inadequate in the others’ presence. Other defenses, such as denial, undoing, or intellectualization, support the primary defenses
Object Relations: issues of autonomy and intimacy, helplessness and hopelessness. There may be an exaggerated dependency on others, and s Sensitivity to criticism and rejection, because he/she is ready to believe the worst about him/herself. fear of abandonment. loneliness. rage and grief. Often stays with an inconsiderate or abusive partner, blaming his/her own inadequacies for the partner’s behavior.
Self: The person has a devalued or distorted self-image; his/her sense of personal value comes from external sources, making the person dependent on the outside world and vulnerable to changes in it. He/she may believe that he/she is bad, for selfishness, anger, envy and other normal emotions.
Antecedents are thought to include…
- conflicts pitting a harsh conscience against a repressed child-representation.
- wishes and fantasied transgressions
- frustrations about being unable to meet ones own high standards
- early deficits of love and affections [MDD,p4,II A2.3]
32b. Treatment Issues
These follow from psychodynamic understanding of the nature of depression.
Identify each issue when it appears in the patient’s narrative, speculate with the patient about its function, use by the patient, specific antecedents, origins, adaptive value, alternatives, and so on; and help the patient find a more balanced understanding of self.
Structural:
Deal with punitive superego by [1] being nonjudgmental; [2] pointing out instances of it as they appear in the treatment [3] thwarting and identifying the patient’s attempts to please the therapist.
Defenses:
Deal with denial.
Object Relations: Explore interpersonal assumptions and reactions, such as…
- reactions to separation, including separation from the therapist, possibly even momentary breaks in the narrative as separations.
- the patient’s assumption that any expression of anger lead to separations.
- idealization of therapist.
- negative reaction to positive feedback from others.
Genetic:
- Ask about history that could have led to any of the above, such as depressed parents, or parents exercised strict control but showed little affection.
- Look for a punitive superego, possibly coming from a precocious sense of responsibility or early demands by parents.
- Listen for a fear of separation and loss, possibly stemming from early losses.
32c. Treatment Techniques and Goals
Treatment involves bringing repressed wishes and conflicts into awareness, where they can be handled openly. Thinking affects feelings and behavior, whether the thinking is conscious or unconscious, but only conscious thoughts can be examined and effectively changed. Similarly defenses.
Often psychodynamic treatment involves and understanding of the ways that unconscious needs and conflicts are acted out in the therapy, because both patient and therapist can then collaborate in observing and interpreting the patient’s “patterns of thought, emotion and behavior”. [MDD,p4,II A2.4]
Techniques are designed to uncover unconscious conflicts or meanings that are affecting present-day life. Once they are brought into awareness, they can be dealt with more directly and effectively.
Help patients become more aware of their own part in creating or interpreting situations that lead to their own unhappiness. This helps empower them to change those situations or interpretations.
There is a range of psychodynamic treatments, from psychoanalysis to brief psychodynamic psychotherapy. They vary according to the extent to which the therapist is hidden or available. Techniques such as remaining out of view, saying little, avoiding self-revealing statements, etc., allow the patient to project his/her internal life onto the therapist. The resulting distortions can be observed and analyzed by therapist and patient together, leading to greater self- awareness. When the therapist is more available as a real person, projections may be less obvious, and technique must be modified to identify the patient’s contribution to his/her difficulties.
—Intensity of treatment. Longer, more frequent sessions tend to produce greater internal material. Shorter, less frequent sessions tend to focus on practical issues and reports of daily living. The assumption of more intense treatment is that the therapist can be most helpful relative to the internal material.
—Duration of treatment. Patients are encouraged to continually bring in new material, and to the extent that they comply, they present a clearer and more complete picture of themselves with the passage of time. This includes material that had previously been out of awareness
—Time limits create pressure and may [1] lead to anxiety that causes the patient to introduce material that might have gone unexamined; or, especially with depressed patients, may [2] reinforce the patient’s expectation of being abandoned by important persons and/or the sense of being pathologically needy and dependent.
Free association has different meanings, depending on the openness and level of intensity of treatment. Generally, a patient is encouraged to let his/her mind wander iin response to stimuli that are very vague in the case of intense, open treatment. [“Say whatever comes to your mind.”] In less intense, more focused treatment, the stimuli may be more specific.
Confronting defenses
Deal with secondary gain from illness, which can include..
- sympathy from others for being depressed.
- being taken care of, etc.
Uncover and interpret unconscious issues as they appear in the patient’s relationship with the therapist and reports of dealings with others in the patient’s life, including…
- excessive dependency.
- vulnerability to loss of self esteem.
- guilt.
32c. Dangers and Limitations of Psychodynamic Treatment
Use of psychoanalytic techniques by untrained or unanalyzed therapists can lead to many risks, notably…
- failure to identify the unconscious roots of the patient’s depression.
- projection of the therapist’s conflicts onto the patient, leading to false attributions of causality and a false illusion of understanding.
Focus on the intrapsychic, the unconscious, and the illogical may…
- neglect external sources of pain and pressure that could be eliminated or reduced.
- fail to address conscious but irrational issues.
- not produce sufficient change quickly enough, and the patient may discontinue before treatment can be effective.
Focus on personality change may be too ambitious for the patient and unnecessary to the treatment task at hand.
Open-ended treatment may extend beyond the patient’s financial limitations, so that treatment can’t be completed in the mandated time frame.
Approach of free association can allow a patient to lose focus and wander along paths that are only tangentially relevant, to repeat endlessly the same complaints, etc.
Concept of technical neutrality may lead a therapist to avoid using other helpful techniques along with intrapsychic exploration.
Psychodynamic techniques often don’t work well with patients who are either not verbal or not psychologically-minded.
32d. Modifications of Technique
Typically psychoanalytic technique is taught as a general approach that can and must be adapted to each patient’s unique personality, conflicts, resistances, etc. Some generalizations are possible:
- Patients whose depression approaches psychosis are generally unavailable to interpretations, and the therapist must focus on management, consider hospitalization or medication, provide additional support, etc.
- A patient who is bipolar and depressed but going into a manic phase also needs additional management and a possible change of medication.