SECTIONS: 5 | 8 | 16 | 19 | 21 | 22 | 24 | 25 | 39 | 44 | 46 | 47 | 48
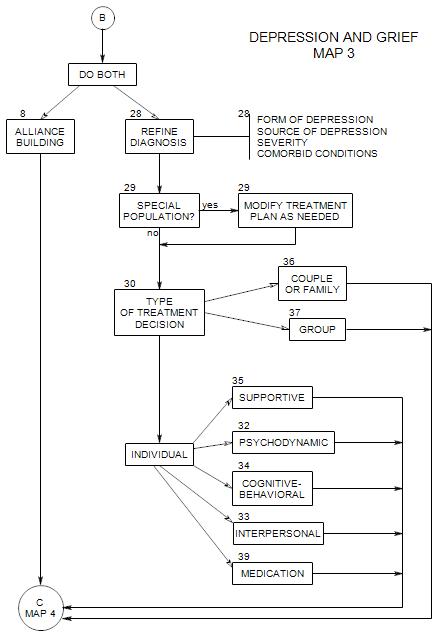
SECTIONS: 8 | 28 | 29 | 30 | 32 | 33 | 34 | 35 | 36 | 37 | 39
-
Coordinates with Section 1 on Map 1A. Appears at the top of each of the other maps. These issues are also discussed more generally in New Patient Section 11.
An alliance is a sense that you are both working for a common purpose, and can help each other do your respective jobs. An alliance not only helps by facilitating the diagnostic and treatment work; it is also part of the treatment, by giving the patient a sense of not being alone, of being able to talk openly and to express his/her thoughts and feelings safely.
FIRST SESSION
You can help the patient feel comfortable, secure, and able to talk with you in a variety of ways:
1. Ask questions that lead the patient to say what he/she wants to say. Usually, this could include the experience of depression, other people’s reactions, his/her theories about the reasons for being depressed.
2. Ask questions that the patient hasn’t thought of but that seem important and related to the problem once he/she does think about them. This could include
- specific symptoms, such as mood cycles, changes in sleeping or eating patterns, etc.
- physical symptoms. Depressed people are often preoccupied with their health and more sensitive than others to real illnesses. Some symptoms may be imagined, many may be real and important.
- when the depression started, and what else was happening in the patient’s life around that time.
- why the patient is here right now: what changed recently that led to this appointment.
- what the patient has done to treat the problem
- any feelings of anger that the patient may have.
This is not only information-gathering; it is also one of the early phases of treatment. By asking questions, you help the patient re-frame the experience of depression, and re-evaluate the causes of his/her mood. [ cf. Section 1 ]
Your main job at this point is to understand the patient and what is leading to the patient’s symptoms, depressive and otherwise.
3. Ask about prior depressive episodes and their treatment.
- When.
- reasons for it/them.
- outcome[s].
4. Ask why the patient came to you. This has several aspects:
- What about the patient’s symptoms led to treatment? [gives information on severity of distress or patient’s symptom tolerance]
- Why now, not a month ago? What changed? [can lead to discussion of severity of symptoms, changes in symptoms, change in life, or change in his/her impact on others]
- Was the patient pressured or coerced to come? [may give information on conscious resistance or interpersonal relationships]
- Why you and not another therapist? this especially if the patient was in prior treatment [may reflect rejection, disappointments, prior success or failure of treatment]
- Who recommended you and what did he/she say about you [gives information on expectations] Why ask that person?
5. Give the patient information about your plan or way of working and what to expect. How much you say will depend on your approach and your sense of the patient’s need to know.
It could include
- the idea that talking can help a person feel better;
- that you won’t be able to tell the patient a lot the first session because you need to learn about him/her first.
- the idea that he/she needs to decide in a first session only whether he/she feels comfortable with you and is able to talk reasonably easily, that you seem to listen and understand.
ONGOING
6. Give the patient some information about depression in his or her context [disease, medications, history]. This can normalize the patient’s situation, offer hope, and be reassuring. It can also show the patient that you have knowledge and sympathy.
7. Consider giving the patient a homework assignment, possibly to explore and keep track of
- mood as a function of time of day.
- antecedents of depressive feelings.
- Dreams.
- other feelings, especially anger.
8. One dimension of process is the extent to which you should make various treatment decisions alone or in consultation with your patient. Issues could include
- the patient’s need to be taken care of and reassured.
- the patient’s need for self-expression.
- the patient’s need for control over his/her own life.