-
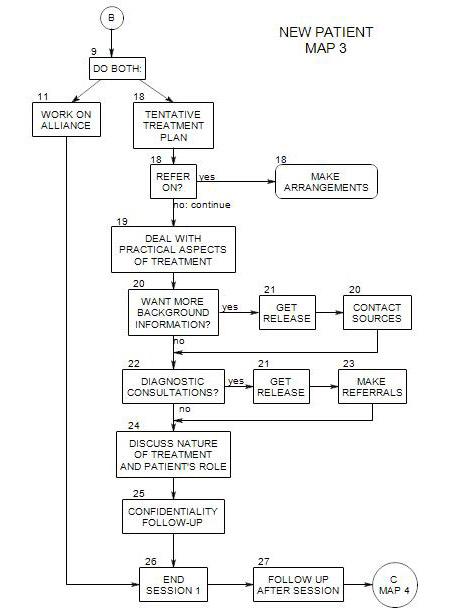
Comes from Map 3
Leads to Section 21: Get Release
This section has to do with deciding what additional information you are likely to want – from outside sources. These choices need to be raised with your patient in session, then your decisions carried out, in Section 27, when the session is over.
A number of people and organizations can provide additional information about this person. You may want to contact one or more, depending on-
- complexity of patient’s issue
- patient’s memory and self-awareness
- availability of test results and other data the patient may not have
Possible contacts include:
- family
- referral source
- physician
- prior therapist or clinic
- hospital or other treatment facility
There are generally both advantages and disadvantages to making each of these contacts.
Reasons for making the contacts:
- to save time in data gathering
- to obtain useful information that the patient doesn’t know or may not choose to tell you
- to get your own impression of the patient’s life context, through meeting with other family members
- to give a (dependent or regressed) patient a sense of being taken care of
- to stay in touch with or to meet other professionals
Reasons for not making the contacts
- to avoid being biased in your diagnostic process. Other family members have their own perspectives on the patient, often based on conflict or conflicting interests. Other professionals may view him/her through the lenses of their own disciplines.
- not to infantilize a patient. Especially early on in the treatment process, you may not be able to predict the person’s interpretation of a request for information from others. He/she may think you don’t trust his/her accuracy of reporting, honesty, etc.
- the patient doesn’t want you to deal with particular people
- the patient may not trust you with some information at this time, and fear you will learn it from others
Note any contact assumes you have obtained the patient’s permission. Most information sources will need a copy of a written release [ Section 21 ].
20a. Discuss the Process with Your Patient
Your patient needs to know whom you want to talk with, the reason for talking with them, and the kind of information you hope to gather.
It would be best if your patient suggested you make the contact. You can ask for suggestions about whom to contact; or you can ask how the person feels about your contacting possible resource people.
If the person agrees, it would be good to have a release ready for signature [ See Section 21 ].
20a. Request Hospital Records
If a patient comes to you following a psychiatric hospitalization, it can be a great saving to be able to make use of information about the patient already collected by the hospital.
Here we are assuming that the patient has been hospitalized for a psychological reason. Some possible reasons include:
- suicide attempt
- severe depression
- vegetative symptoms: not eating or not sleeping
- drug abuse
- bipolar disorder
- borderline personality with suicidal gesture
- schizoaffective disorder
- organic brain syndrome
During the patient’s stay, the hospital staff may have gathered or generated information about past history, prior hospitalizations, current and prior medications, diagnosis, response to treatment, etc.
It may pay to be in touch with a particular person at the hospital, especially if you already know that person. They can possibly expedite the flow of information, put you in touch with the patient’s therapist for clinical impression, etc. And it can help to stay in touch with your contacts.
It is best to ask for the entire treatment record: medications, history, etc.
A difficulty can be obtaining the information in a timely manner. The hospital will need a release from the patient or a relative in order to send it to you. This could take time, especially if you wait to get the release until the first session with the patient.
A quicker way would be to ask the patient to bring records to your first session with him/her, or to send the hospital a release that specifies you to receive the information. However, with many patients this may not seem appropriate to discuss in an initial phone call.
When a patient is referred by a hospital, records may be sent to you as soon as you accept the referral, or you may have to request them.
20c. Contact Patient’s Insurance and Managed Care Companies
Section 19 includes a list of information you should collect from the patient in order to deal with his/her insurance and managed care companies, along with a map, Dealing with Fees.
If the person has brought an insurance card to the first session, you can get his/her plan name or number, the name he/she uses for insurance purposes, and an insurance contact phone number. Save that information to use in contacting the insurance company.
From the insurance company, you need to verify
- that the patient is covered for your services.
- the maximum number of covered sessions per year. This may depend on the patient’s diagnosis and type of treatment.
- procedures for being paid. Some companies use special forms for claim approval and submission. Others use a standard HCFA. Procedures for filling out claim forms may also vary from company to company. Currently, more and more insurance companies prefer electronic claim submission and payment, but they may grant exceptions for small practices.
- allowable copayments. If the patient is in a managed plan, the copayment may be fixed.
- the amount of reimbursement per session.
- the claims address.
If the patient has managed care and you are a participant in the patient’s plan, you need to know the procedure for obtaining approval for continued treatment
Also if the patient has managed care, you should make a note from previous experience with the company or consulting with colleagues the number of sessions that the managed care company is likely to approve. This may be fewer than the number of covered sessions, and can have a serious impact on your treatment plan for the patient.
If the patient doesn’t have managed care, or if you don’t participate in his/her plan, then you will need to negotiate the fee.
20c. Contact Patient’s Prior Therapist or Clinic
Sometimes this can be very helpful, especially if the patient perceives the prior treatment as having been successful. You must decide whether the previous therapist’s impression of the patient can be useful to you, or whether it can limit your own impression.
However, if the patient sees the prior treatment as unsuccessful or didn’t like the therapist, he/she may oppose your making the contact.
20d. Contact Referral Source
There are at least three reasons to contact the person or institution that sent the patient to you or gave the patient your name:
- to let them know that the patient is being treated
- to learn more about the patient
- to thank them for the referral
If you plan only to call or write to acknowledge the referral, you should first discuss it with the patient. The patient may have good reasons not to want you to do so, [including the possibility that others in the family of the referral source could find out, etc.].
If you may also use the referral source as a source of information about the patient, you should obtain a written release before making the contact.
20e. Insurance or Managed Care Referral
In this case, contacting the insurance or managed care company is often necessary in order to begin treatment. Refer to your contract with the company. Then see Section 19 about dealing with insurance and managed care companies.
20f. Talk with Other Family Members
Family members can give you information about
- the patient’s place in the family [scapegoat, sensitive one, in conflict, dependent, responsible for others, awkward, distant]
- environmental stresses the patient may be experiencing and have failed to mention
- typical family interaction patterns [blaming, affectionate, arguing, withdrawing, confiding in each other or not]
- reactions of others to the patient
- their assessments of the patient’s problem [depressed, awkward, angry, rejected]
- possible physical sources of the patient’s symptoms or concerns
- other possible sources of the patient’s issues
- patient’s psychological or behavioral history
- reactions of family members or friends to the patient’s behavior and symptoms
- others in the family with psychological histories
Meeting with other family members can also suggest directions for treatment:
- form of treatment [possibly: couple or family therapy, to change interaction patterns]
- severity of patient’s disturbance
- likelihood that patient will carry out the treatment plan
- using other family members to assist with the patient
- whether to focus on the patient’s disturbance directly or on some likely source of it
- whether another family member should be in treatment [for his/her own issues] or counseling [re contributing to the patient’s issues]
20g. Patient’s Physician.
You should consider consulting with the patient’s internist
- as part of an initial diagnostic process
- regarding ongoing medications
- with questions developed during your information-gathering]
If the patient’s physician made the referral, you will want to know why. Often physicians refer when the patient’s symptoms are bizarre or clearly psychological, or when medical treatment has been ineffective, or when the patient has been noncompliant with medical treatment, and sometimes just because they are tired of dealing with the person.
You will also need to know what treatment choices the physician has made that could affect your work. [prescribing an anxiolitic or antidepressant; giving advice about the patient’s issues, etc.], including prior medical interventions.