-
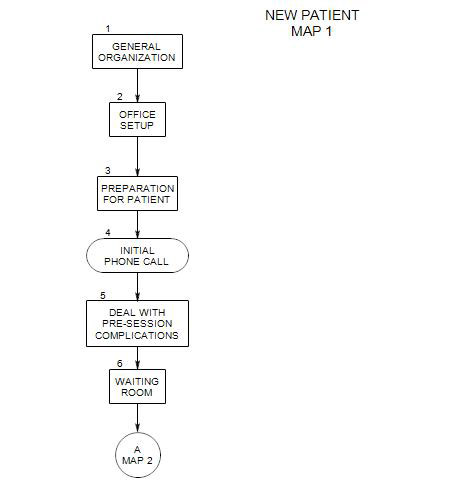
Follows Section 2 on Map 1
The following section attempts to combine basic ideas about preparation for a patient with legal requirements of the Health Insurance Portability and Accountability Act [HIPAA].
3a. Preparation for Initial Phone Call
You need to be ready for an initial call from a prospective patient, both when you actually receive the call and when you are not available.
A person may call when you are unable to answer for a variety of reasons. You may be away, in session, asleep, on another line, etc. In this case the person will need to leave a message, so you can return the call. Then
- A decision has to have been made, about whether to use an answering service, use a call recording service from your telephone provider, or have an answering machine.
- In either of the first two instances, you will need to make sure that the information recorded and forwarded to you remains confidential. The message company is considered an associate of yours, and you will need to have written assurance of confidentiality from them.
- In the third case, you will need to be sure that access to the information left on your machine is available only to persons who will maintain confidentiality, and that no one can hear the message coming in who should not hear it.
It is a good idea to check for messages frequently and return them promptly. People tend to call only when the need becomes great enough, and a quick response is important to them.
There is another reason to return initial calls promptly: often a person will call more than one therapist, and the first to respond has the greatest chance of making an appointment. A person who has made an initial appointment with one therapist is far less likely to schedule an appointment with the next therapist who calls back – unless the appointment with the first one is disappointing.
When you return the call, you should be ready with your schedule, a rough idea of how much information you want to provide over the telephone, a list of insurance plans you accept, and anything else that is likely to be important to a potential patient.
If you actually pick up an initial call from a potential patient, you should also have the same basic information available, or be prepared to explain that you don’t have your calendar handy, etc., and let him/her know when you will be able to provide the missing information.
3b. lnformation to Have Available for an Initial Session
It is helpful to have the following information available:
- Insurance plans you accept, and their deductibles, annual and lifetime caps, and expected reimbursement rates. If you participate in managed care plans, you should be able to tell a prospective patient the mandated copay and likely number of reimbursed sessions as well.
- Names and telephone numbers of other therapists that you can refer to, in case you are unable to see the patient yourself. Ideally, you will know each of the therapists you recommend, their personalities, their ways of working, the kinds of insurance they accept, etc. It can also be helpful to know whether they are available and if so, when they have open hours.
- Names and telephone numbers of low-cost clinics, and some knowledge of their intake policies and procedures. Some idea of length of their waiting list can also be helpful.
- Hospitals and their procedures for hospitalization. It can also be helpful to know people on staff there, as an aid to securing admission.
3c. Gathering Protected Health Information [PHI]
HIPAA defines Protected Health Information as any information about a person that identifies the person, is private, and is necessary for providing treatment.
You should have some way of recording-
- personal information: name, address, telephone number
- contact information: name, address and phone number of physician, relatives, etc.
- billing information: Who pays, and what part. If managed, contact information and procedures. Fee. You may want to have billing software in place.
- medical information: any prescription drugs, amounts and times taken. OTC meds: what, when taken, amounts
- physical disabilities or other information that could bear on symptoms
- diagnosis for insurance purposes
- patient’s level of functioning; your treatment plan if any; prognosis, symptoms, and progress.
You also may need to gather and record more or different information [eg: date of birth and insurance identification number] if you are billing a third party for payment. If you like forms, you may need different forms for different situations [patient pays each session; insurance is billed first and patient has a copay; patient is billed monthly and forwards a statement to his/her insurance company; etc.] You should have ready
- Release forms for the patient to sign, that state the terms of information exchange with family, friends, or other professionals
- Insurance claim forms [esp: HCFA] for patient to sign
- Your appointment calendar
- Notice of Privacy Practices [HIPAA]
3d. Therapy Notes
Psychotherapy notes are defined by HIPAA as the personal and intimate information about patients that are not needed for treatment authorization or basic record keeping. They can include session notes, reports of dreams, your reactions to the patient, etc.
Although psychotherapy notes are part of a patient’s Protected Health Information, they have a different legal status from the remainder of PHI. The patient doesn’t have a right to see them without your permission. However, you also may not share them with anyone else without the patient’s permission.
3e. Assuring the Confidentiality of Records
At one time this was primarily an ethical [the patient has a right to privacy] and practical [a patient may be reluctant to talk about issues that could become public] matter. Now there are laws about confidentiality at both the state and Federal level, that set minimal legal standards for how you can treat the information people tell you about themselves and others.
In addition to your own professional standards, you need to comply with the HIPAA and your state’s confidentiality laws. In case of a challenge to your treatment of patient information as confidential, the more stringent [HIPAA or state laws] will apply.
This means-
- preparing a folder that tracks your HIPAA compliance activities.
- having HIPAA forms available for use with patients; especially the Notice of Privacy Practices, Authorizations, your disclosure log, and the forms to request that health records be amended.
- keeping therapy notes separate from Protected Health Information.
- making sure that the physical set-up of your office and any other place you discuss patient information is safe from being heard by anyone who does not have explicit patient authorization.
- having a place where all hard copies of information about patients can be locked away.
- providing security for any computer records about patients.
- if you bill electronically, making sure that the system you use is HIPAA compliant.
- making sure that any business associates who have access to patient information [including insurance carriers] are also HIPAA compliant.
- posting a notice of privacy practices in your office or waiting room.
If you are not currently HIPAA compliant, you can get information about it from your professional organization, or take a course in it for CE credit.